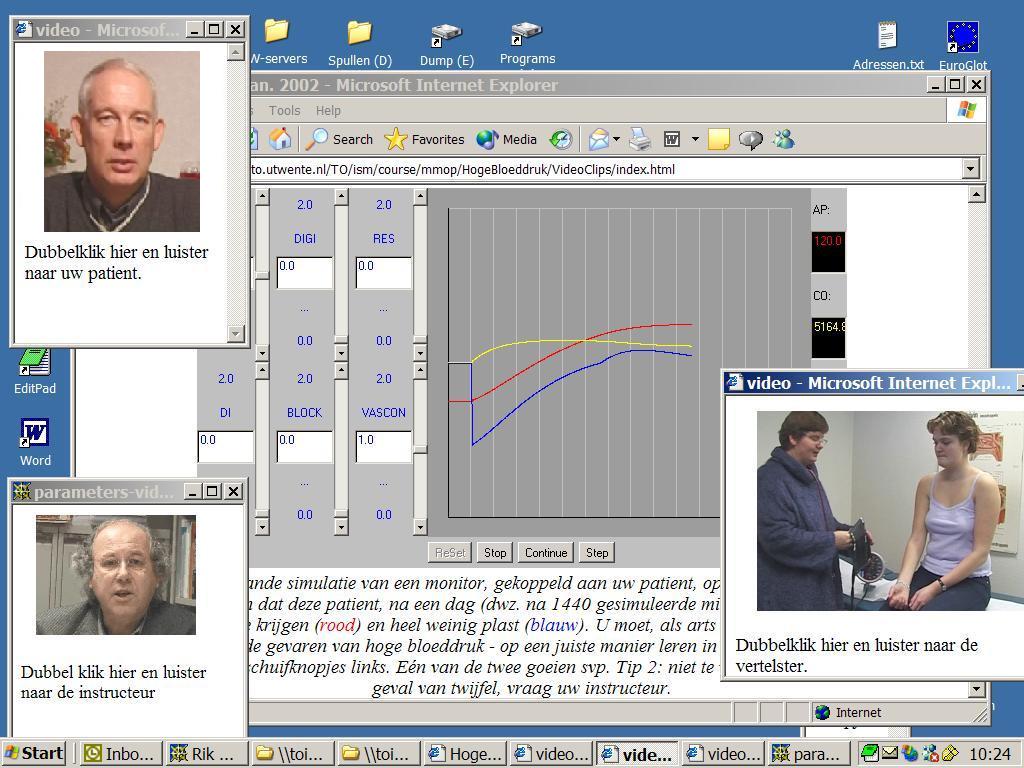
Figure 9.1. Screendump of one of the first versions of the computer simulation program CARDIO (version 3.1). You see output and input-possibilities of and into the blood pressure in a human body [circa 1990].
This chapter covers:
This chapter presents the model, possibilities and results of or with CARDIO, a simulation program on blood pressure regulation under normal and abnormal conditions. The model underlying this program allows the simulation of pathological conditions, such as myocardial infarct, renal artery stenosis or renal insufficiency. Therapeutic interventions in abnormal conditions can also be simulated. The program allows the application of drugs like cardiac glycosides, diuretics or vasodilator.
The computer simulation program CARDIO enables students to experiment with the basic principles of blood pressure regulation for a healthy young man. The program simulates an experimental laboratory where hemodynamic research can be done, variables can be registered, and where interventions in the model can be made without real-life complications. The computer simulation program CARDIO is often the first moment in the curriculum in which the student can check his or here understanding of human circulation in the context of realistic problems. With this computer simulation program the student can do a series of experiments, such as the simulation of heart failure, hypertension, renal failure, exceptional blood loss, selective venous constriction, and selective arterial constriction.
These interventions can be selected by the student or chosen as a case by the teacher. When it is presented as a case the student can be asked to form a diagnosis and operate therapeutically, starting the hemodynamic picture on the graphical screen. The student has the possibility to introduce medicines like heart glycoside (digitalis), vasodilator, diuretic, sympathicolyticum, or noradrenaline.
The model of the computer simulation program CARDIO is based on a model of Coleman (1980) of the cardiovascular system of a healthy human being. It consists of five compartments: the heart, the vascular system, the intra- and extracellular fluid volumes, the nerve reflex system, and the kidney. The model contains a number of relations between parameters in these compartments and consists of about 60 variables.
Coleman's model of the blood pressure regulation and the cardiovascular system distinguishes three important regular quantities:
1. The extent of the vascular resistance is chiefly determined by metabolic and neural factors. In this way it is possible to keep the circulation of blood within the different tissues in the model as constant as possible (auto regulation) while adapting to system needs. The preservation of the flow within a number of tissues is one of the most important cardiovascular physiological priorities of the intact organism.
2. The mean arterial pressure is acutely regulated by the nerve reflexes, notably the baroreceptor reflex (blood pressure regulation by the renin-angiotensin system is not included in CARDIO). In the long run blood pressure is regulated by the kidney function which controls the extracellular fluid volume.
3. The cardiac output is primarily determined by the venous return. Moreover the cardiac output can be directly influenced by the function of the heart as a pump.
Figure 9.3 contains a graph of the most important relations in the model. The interventions which are possible in this model and their points of application are mentioned in it. The most important variables of the model and their normal values are:
The model contains possibilities for changing the physiological situation or making this cardiovascular system ill, as:
The model contains 'medicines', as:
The model underlying the computer simulation program CARDIO was further developed from Coleman's model and tested at the University of Limburg at Maastricht with the RLCS system and later on at the University of Twente with the computer simulation system MacTHESIS. The description of this model will be discussed relative to Pascal notation and to analogue notation, as well as to the manner in which these notations complement each other.
The heart
In the model the basic Cardiac Output (COB) -- i.e., the cardiac output without the influence of the autonomic nerve system -- is a function of the right atrial pressure (RAP). The cardiac output (CO) is determined by the basic cardiac output (COB) and a heart function parameter (HF). This heart function (HF) is a function of the right atrial pressure (RAP), the mean arterial pressure (AP), the sympathetic nerve activity (AO), possible cardiac glycoside (DIGI), and the basal heart strength (HSB).
The circulation
Many tissues in the body function optimally when the flow through the tissue of the organ remains constant within certain limits. The regulating mechanism that controls this tries to realize it through changes in the resistance. In this model an attempt has been made to include an overall description of the autoregulation phenomena. The mean arterial pressure is the product of the total peripheral resistance and the cardiac output:
AP: = CO*TPR;
Intra- and extracellular fluid volume
The extracellular fluid volume (ECFV) is directly influenced by the fluid volumes which are taken in by the body minus those which leave the body:
ECFV: = ECFV + (WIN - UO - BL)*dt;
In the model ECFV(0) = 15000 ml and the intake and output is 1 ml/min. The water intake of the body (WIN) is set to 1 ml/min. The urine output (UO) is 1 ml/min and the loss of blood (BL) is normally 0 ml/min.
The nerve reflex system
The autonomic nervous activity (AO), the value of which in the normal situation is adjusted to 1, is dependent on the chemo and baroreceptor activity, a possible adrenergic blockade (BLOCK), a possible pheochromocytoma (PHEO) -- which develops an excessive sympathetic activity -- and a possible alpha-adrenergic influence of norepinephrine (NOREPI).
The kidney
The kidney function depends on the composition of the blood, aldosterone, neuronal factors, angiotensin, vasopressin, and the mean arterial pressure. In this model the basic urine output (UOB), normally 1 (ml/min), is a function of the mean arterial pressure (AP), the basal renal arterial resistance (RARB), the autonomic output (AP), and a vasodilatation factor (DILAT).
The complete model written in Pascal is given by Moller and Van Wijk van Brievingh (in press). In their book an executable MS.DOS version of CARDIO has been enclosed.
The normal values for the mean arterial pressure (AP), the cardiac output (CO), the total peripheral resistance (TPR), the urine output (UO) and the heart frequency (HR) in the computer simulation program CARDIO, with the given aggressive values and without any intervention are: AP =100 mmHg; CO=5000 ml/min; TPR = 0.02 min.mmHg/ml;
UO =1 ml/min and HR =70 min.
These 5 important hemodynamic variables can be supplemented by the extracellular fluid volume (ECFV), the blood volume (BV), or the pressure of the right atrium (RAP). These variables are normally not easy to measure. In the exercises described here such variables play an important role. The computer simulation program CARDIO not only gives visual feedback on the student interventions but also textual feedback.
The following messages can appear on the screen when a particular variable reaches above or below a certain limit:
In one version of the computer simulation program CARDIO these texts were given in audio fashion using audio technology. In an other educational environment on the web you see a video version with a 'talking head' with this intelligent feedback ('ICS') (see also figure 9.2 and 9.8: two versions of 'Maurice') (Min, 1999 - 2004). In the visual output, the head of the 'simulated patient' leans to the left if the 'simulated patient' dies.
Heart failure
In figure 9.4 the hemodynamic effect is simulated of a light heart failure. In the point of time as shown in the figure the contraction strength of the heart muscle is reduced by 30% until 70%. The cardiac output decreases sharply while the baroreceptor reflex mechanism tries to compensate the fall in blood pressure. This activity can be seen from the increase of the heart rate.
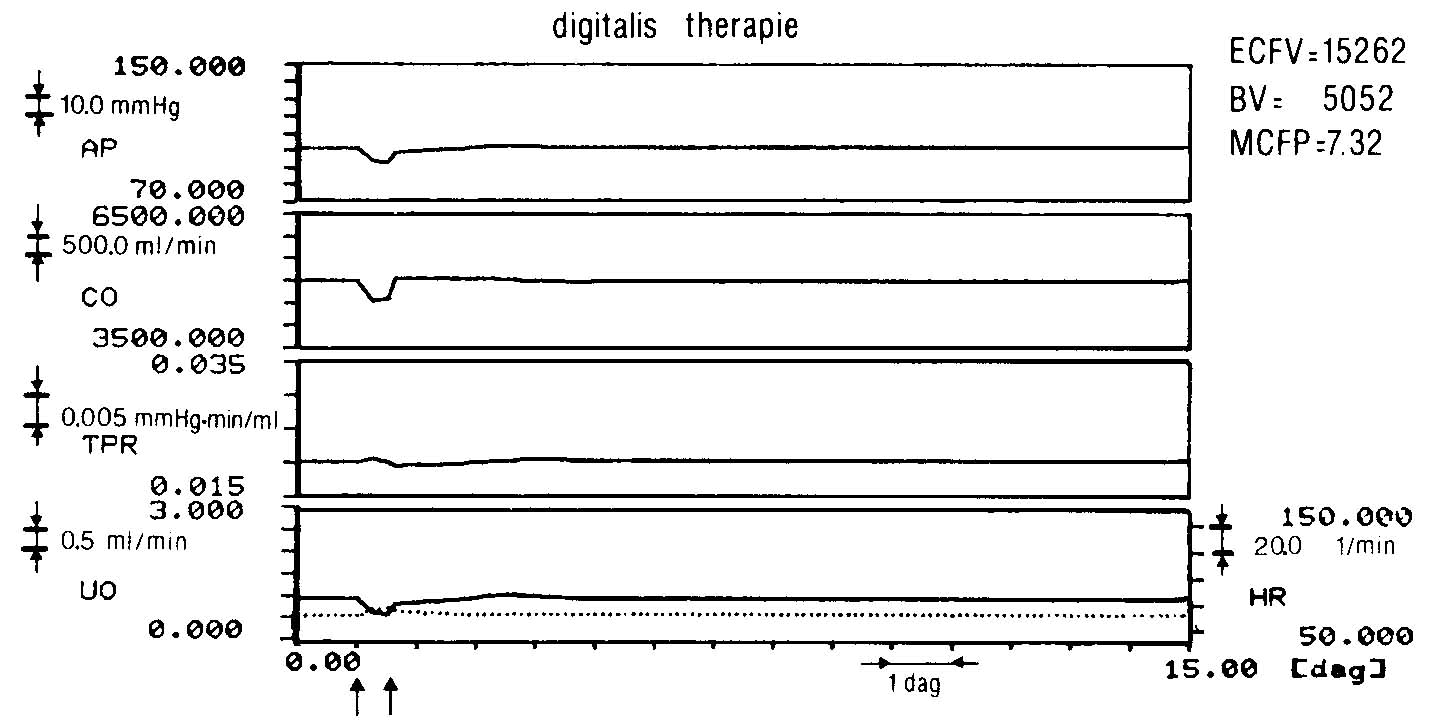
If the simulation is continued there are no significant deviations to be found after two weeks in a number of measured and registered variables. However, other variables do change. Careful analysis of the simulation data with the inspection options shows that there is renal retention of fluid. After 14 days the ECFV has risen to 17000 ml and the blood volume (BV) to 5400 ml. Thus the inability of the heart to pump an amount of blood adequately per time unit is compensated by an overfill of the vascular system by which the cardiac output keeps its normal value. In reality this also happens in case of a light heart failure. We then speak of a 'compensated heart failure'. By this is meant that the heart function is restored in spite of the diminished contraction strength of the heart muscle. When the student intervenes in the model shortly after the compensation power of the heart muscle has diminished by 30%, a digitalis therapy can be started which can prevent the overfill of the vascular system and by its primary effect, intensify the contraction strength of the heart muscle. After a short while all variables appear to have returned to their normal values from before the sudden heart failure. With a careful dosage of digitalis (DIGI is about 0.6 units), the condition of no significant increased ECFV and BV and a normal right atrial pressure (RAP = 0 mmHg) can be achieved.
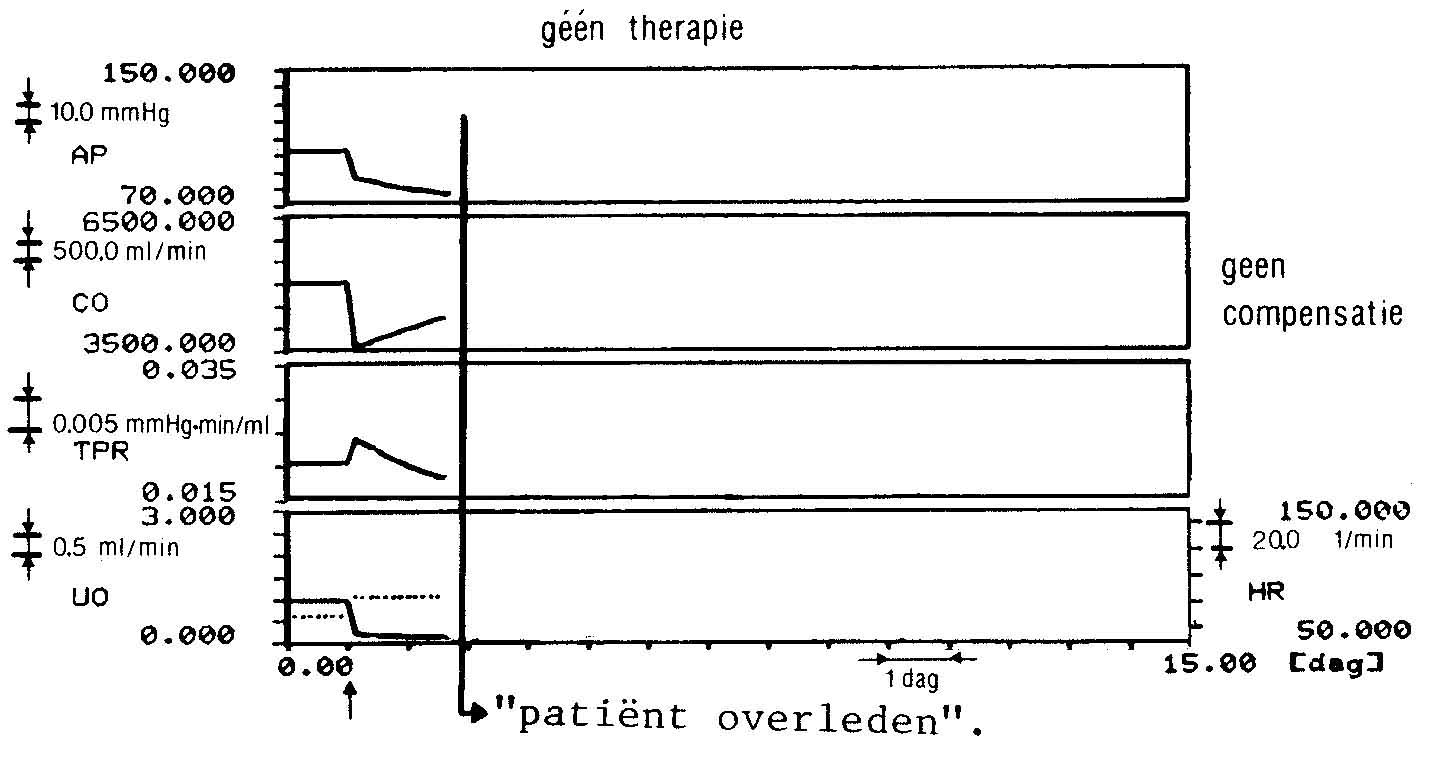
In Figure 9.5 the hemodynamic effect of a severe heart failure is simulated. At the given point of time the contraction strength of the heart muscle (HSB) has diminished by 70% to 30%. The cardiac output drops much faster than in the first case. The reflexive increase of the peripheral resistance and the fall in urine production is also sharper. If there is no therapeutic intervention, a patient with this hemodynamic pattern will soon die of the type of suffocation which can occur due to pulmonary oedema.
If the student intervenes in the model shortly after the moment when the heart insufficiency occurred and he begins a digitalis therapy (DIGI > 0), he may save the patient from possible oedema. A diuretic can also reduce a possible increase of the extracellular fluid (DI > 0).
Finally, the student can also experiment with a vasodilator (VASCON) in this simulation, together with the digitalis therapy (DIGI).
Hypertension
Figure 9.6 shows, a constant high blood pressure due to a renal arterial constriction (RARB = 1.2) initiated after 7 days. This is a simulation of a renal artery stenosis. The excretory function of the kidney decreases and fluid retention occurs. The mean arterial pressure (AP) rises due to the increased cardiac output and via autoregulation a rise of the total peripheral resistance (TPR) is caused. After 7 days the variables are: AP = 120 mmHg; CO = 5100 ml/min; TPR = 0.023 min.mmHg/ml; UO = normal and HR = normal.
The student can treat this form of hypertension, due to renal artery stenosis, with three anti-hypertensiva or a combination of these. The program has the possibility of:
The influence of the dose is shown in some dose-response curves in the case studies in the student manual.
Figure 9.6. Case of hypertension. On day 1 RARB, renal arterial constriction, becomes 1.22. After six days the mean arterial pressure (AP) is 120 mmHg and the total peripheral resistance (TPR) has increased to 0.0235 min.mmHg/ml.
Hypertension can also be simulated by acute kidney insufficiency (lower renal mass (RM) to 10%) or by a pheochromocytoma (PHEO). However, this case is limited to renal artery stenosis. In case the student chooses a diureticum as anti-hypertensivum he or she has to choose for DI = 1, which will make the patient normotensive (100 mmHg) after about 2 days.
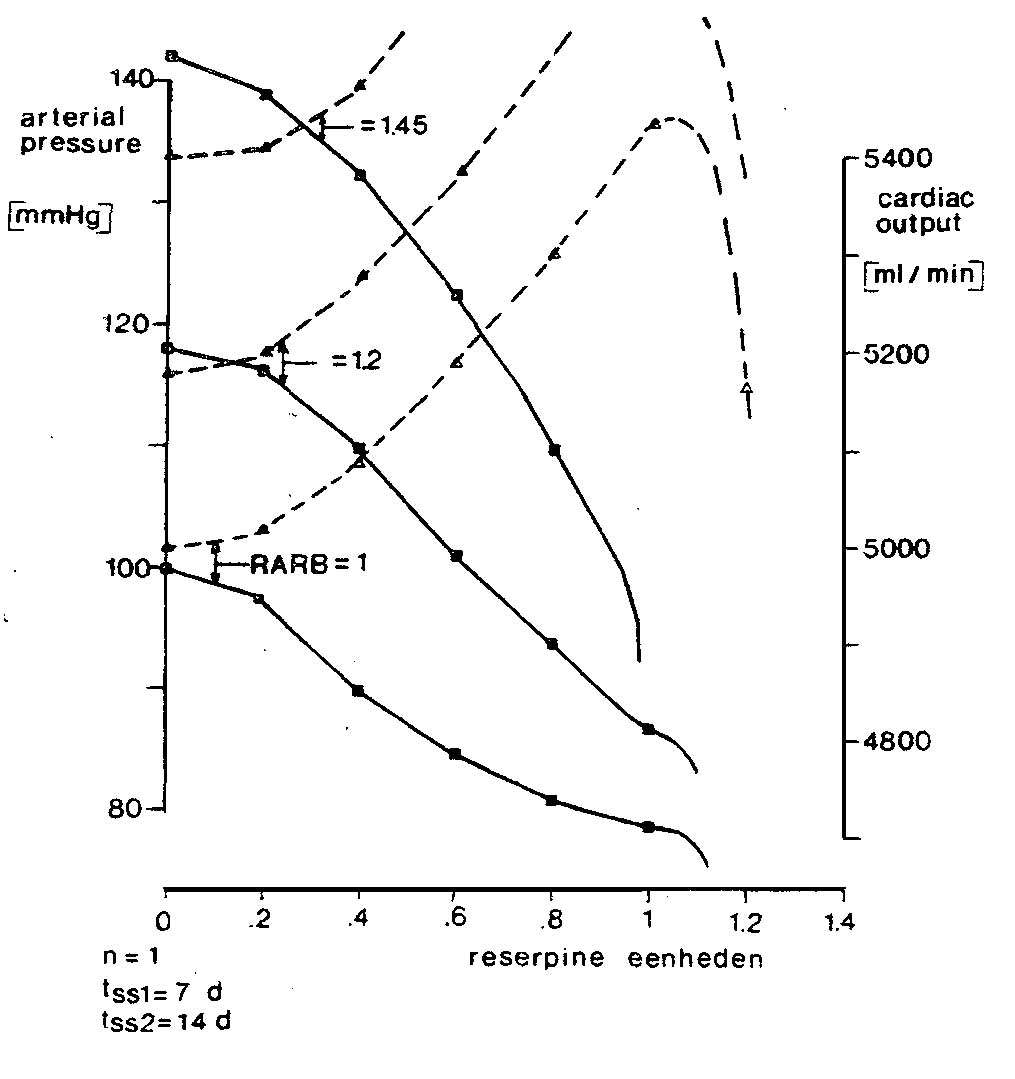
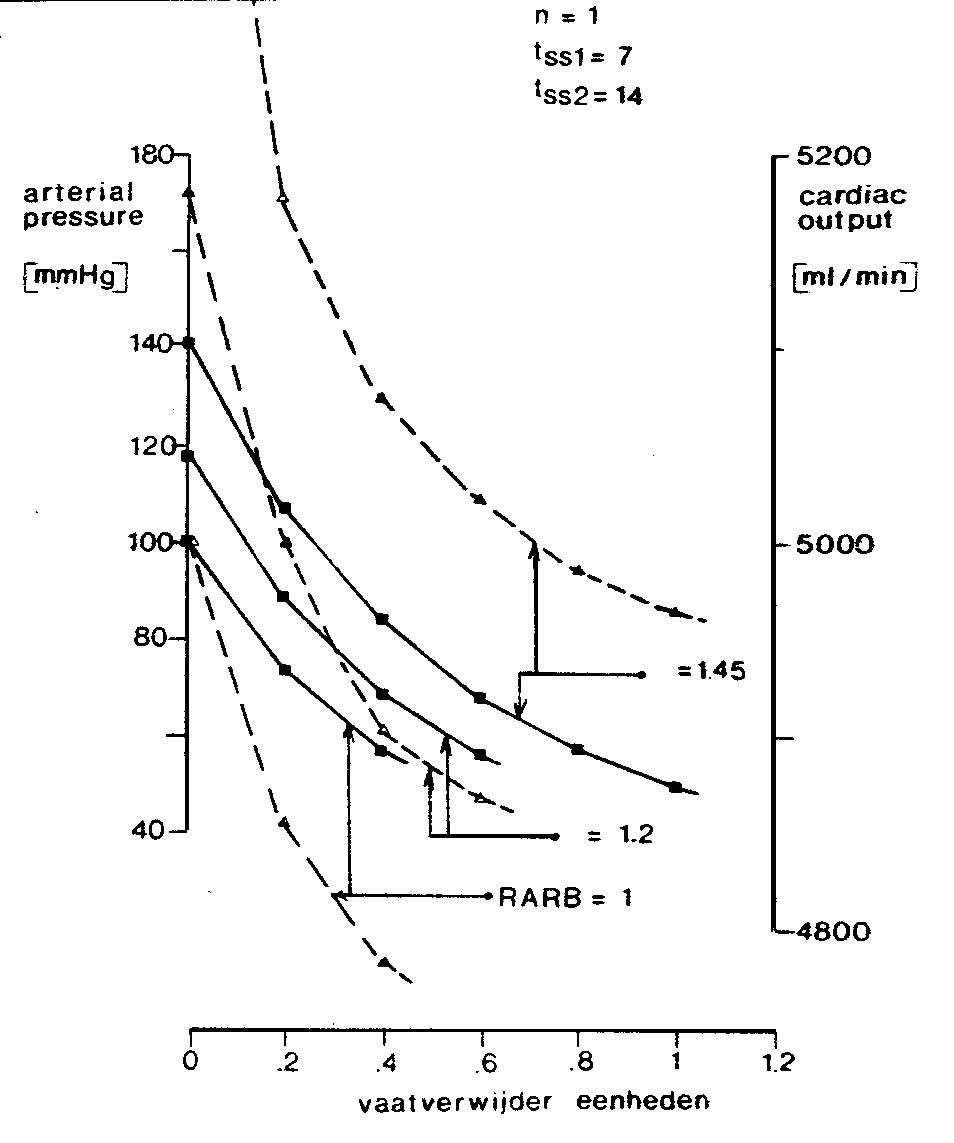
If the student choses a vasodilator which does not effect the kidney, VASCON = 0.15 is sufficient to keep the blood pressure normal for a few days (AP = 100 mmHg). The cardiac output is then increased. However, it does not lead to a permanent fall in blood pressure. With a sympathicolyticum as anti-hypertensivum (BLOCK = 0.65) is sufficient to normalize the blood pressure after seven days. The cardiac output is then considerably increased to 5400 ml/min.
The model of the computer simulation program CARDIO is one of the first to be implemented in the RLCS-system of the University of Limburg in Maastricht and in the MacTHESIS system of the University of Twente.
With this computer simulation program, experience is acquired in certain curriculum blocks, namely, in the block 'heart and lungs', in the block 'fatigue', and in the block 'pain on the chest'. Causal relationships, within cases regarding to heart failure, hypertension, and therapies for various afflictions, are developed by several students working together. It proved necessary to put it in the form of a patient case, since the average time of two hours in which students use a computer simulation program in a block, they can only put one or at the most two problems to discussion. The cases 'light' and 'severe heart failure' usually make them look up in books how the body can compensate a heart insufficiency by retaining fluids. If the 'digitalis therapy' is not applied or insufficiently so, the student runs the risk of getting the message that the patient has 'swollen feet' at a certain moment.
The case 'hypertension' often induces the student to study the working mechanisms of antihypertensiva more closely. An important aspect of this case is that the student also learns how to handle some aspects of relationships between working doses of antihypertensiva and that vasodilators cannot function chronically as a mono-therapy for hypertension.
The computer simulation program CARDIO has had various versions, a great deal of experimentation has been done particularly with the two-terminal versions. It has also been frequently demonstrated to external and internal experts in order to stimulate discussions and opinions about the design of the system (Min, 1982).
The program has been used by several generations of students at the University of Limburg at Maastricht from May 1980 until now (1991). In 1987 there were in all 3000 student sessions with the computer simulation programs CARDIO and FLUIDS on the RLCS-system (with two monitors). Other universities in Europe use other versions of CARDIO but the extent of this usage in their regular curriculums is not known. The computer simulation program CARDIO has versions on PDP11/03 (MINC computer) (the RLCS-system), VAX 11/750 (THESIS, VAX version), Macintosh (MacTHESIS), MS.DOS (THESIS system, MS.DOS version) and Atari 1040 ST with the 'Alladin' or the 'MacBongo' Macintosh emulator. The University of Amsterdam, medical faculty (AMC), uses the model of CARDIO on MS.DOS computers, built through a student of the University of Twente, without one of the simulation systems of the THESIS family, and without multi-windowing. It is used by 250 students in physiology now.
Min, F.B.M., (2004)
Designing Dynamical Learning Environments for Simulation: Micro-Worlds &
Applets on the World Wide Web; In: Instructional Design for Multimedia Learning.
Waxman Munster/New York/Munchen/Berlin. p.57-69. (Eds. Helmut Niegemann,
Detlev Leutner and Roland Bruncken). ISBN 3-8309-1384-2.
Min, F.B.M., (1996)
Simulation Technology & Parallelism in Learning Environments; Methods, Concepts,
Models and Systems. Publisher: Academic Book Center, De Lier. ISBN 90-5478-036-3
Min, F.B.M., (1993)
Biomedical Modelling and simulation on a PC; A Workbench for Physiology and Biomedical Engineering (3 chapters). Springer-Verlag New York Berlin; (Editors: R. van Wijk van Brievingh and D. Müller).
Min, F.B.M., (1989)
De rol van Object-georienteerde talen voor Computersimulatie; Inventarisatie van ervaringen met talen als SmallTalk en Prolog om Intelligente Computersimulatieprogramma's, 'ICS', te kunnen ontwikkelen; Rapport Studiereis USA, maart 1988, Internal publication in the 'ISM informatie reeks' (89.21), Universiteit Twente, Enschede.
Acknowledgement
The author gratefully acknowledges the contribution of dr. T.G. Coleman, University of Mississippi, USA to the computer simulation program CARDIO.
Note
A listing of the model, in Pascal, is published in Mller, D., and R. van Wijk van Brievingh (Editors), Springer Verlag, Berlin (1993). (included the simulation program CARDIO, MS-DOS version)
Note
The oldest, extended version of this chapter, first published in Dutch in: Min, 1982; Ph.D thesis, University of Limburg, Maastricht and in English in: Mller and Van Wijk van Brievingh, editors; Springer Berlin (incl. 6 floppy disks).
Note about the figures:
See them all of better quality in the real existing book: Rik Min, Simulation Technology & Parallelism in Learning Environments; Methods, Concepts, Models and Systems. Publisher: Academic Book Center, De Lier. Holland. ISBN 90-5478-036-3 (1996).
